What to do with a Shifted Spine
Have you seen this before?
Corey depicting a lateral spine shift.
I have had multiple clients with the same presentation where they came in feeling “crooked”, “shifted”, “not right” or “my back is out”.
It is most commonly called a lateral shift. But it has other names such as sciatic scoliosis, trunk list, acute lumbar/sciatic scoliosis, wind-swept spine or lateral deviation.¹ Have you seen this before? Do you have a friend or family member that has suffered from this? If you aren’t sure, here are some key things you can look for.
Some, but not all of the following symptoms may be present:
Your upper body is shifted to one side and hips the opposite direction
There is local back pain that is sharp or achy
A muscle spasm is present in the lower back
You may have difficulty correcting the shift by yourself
It is hard to bend forward or backwards
You cannot sit for too long
You may or may not have pain, tingling or numbness down one of your legs
This may have happened before, or it’s the very first time
When lying down on your back, the shift goes away
You have to lean on one leg to get relief
Okay, I have this condition, what do I do to find pain relief?
The initial goal is to decrease irritation of the lower back. We use the phrase – do not poke the angry bear! Avoid movements that produce back pain initially. From the start of the injury, inflammation usually lasts for 3-10 days depending on the severity of the injury. Your doctor may prescribe medications for relief that may or may not help. The other option is to find the right positions for your back to decrease irritation of the structure causing pain.
Here are some common positions that might be helpful if you have this condition.
Lying on your back
One option is to rest by lying down. A common presentation seen with this type of problem is that the shift disappears when you lie down. The most common position that feels comfortable is to lie flat on your back. I have had clients of mine putting pillows underneath their legs to relieve pain. You will find that if you are shifted and bent forward slightly due to pain, that pillows under the knees will be helpful temporarily. Otherwise, lying on your back with your legs straight may be best. Your pain relief will not be perfect, but it should relieve some pressure nonetheless. Ultimately, you will need to find a clinician to help correct the shift in your spine. Lower back traction may also be helpful but the affects will be very transient. In some cases, traction can worsen symptoms. So be cautious if you are getting your family member to pull your legs or if you’re looking up Youtube videos showing how to self-treat at home.
Standing is your best friend
Corey using a step stool to provide relief from leg pain while standing.
It is important to not sit for too long as sitting most commonly worsens this condition. Standing may be your best option. Again, it will only provide temporarily relief. It is imperative to cycle between lying and standing. If you have leg pain while standing, place the painful leg on a step stool. Again, this will decrease your pain, but will not be the permanent solution to your problem.
Will acupuncture or dry needling help?
It may help, but in my experience, the relief will be temporary. The muscle spasm in your back will release with acupuncture or dry needling, but with standing or walking it will slowly come back. The muscle spasm is present because it is protecting the injured area. Therefore, releasing muscular tension may aggravate the symptoms in your back or leg.
Acupuncture may help with nerve-related leg pain, so it may be a good option initially when you are in a lot of pain. But this will not provide the permanent solution. Movement will be the best medicine for this condition and it is important to find someone who understands the patterns you are reporting.
What causes this condition? Why is my back shifted?
Usually, it is an event where you are twisting and bending forward to pick something up. It could also be brought on with gradual load of your spine when sustaining a slumped posture. It could also be precipitated with lifting something extremely heavy that is beyond your spine’s capacity to handle.
There is speculation on what is being irritated in your back structurally. Your back is shifted because it is a protective mechanism that your body adopts to protect structures like a nerve. If a nerve is irritated from a back injury, your body will naturally shift away to create space so there is decreased compression of the nerve. This would explain why some of my clients would have tingling in their leg initially, plus a shift in their lower back.
Another theory purported by researchers is a disc protrusion or disc herniation resulting in a shift of the lower back. The disc pushes out laterally or to the side, causing the body to shift away from the protrusion. This would explain why some clients will have a shift, but do not have leg symptoms and just local back pain.
Is it something serious?
The key questions I will ask my clients to see if they need to seek immediate medical attention are:
Have you lost bowel or bladder control?
Have you lost the urge to urinate? i.e. you cannot urinate anymore or are retaining urine
Have you lost sensation in the area where you would wipe after going to the washroom?
For males - have you experienced sudden erectile dysfunction?
Do you have lancinating pain in both legs that does not change with position?
If you have said yes to any of the above questions, it would be important to head to the emergency room. If you are receiving help from a health care professional, ask them to write down the findings on a note for you to take to the hospital.
I answered no to all the questions above but I still need help… do I need surgery?
No! In fact, if you answered no to the questions above, there is hope! Most lateral shift cases can be resolved with movement thankfully. The most well-known method used to treat this condition is called the McKenzie Method or Mechanical Diagnosis Therapy. It is a systematic approach which repeats movements of the spine to look for patterns that will guide you towards recovery. For example – your physiotherapist will try to correct your shift. During the correction, they will ask how the symptoms in your back or leg feels. Afterwards, they will check to see if your range of motion and strength change afterwards. If strength and range of motion improve, this indicates that things are trending towards improvement. If you experience a loss of motion and weakness in your leg, this indicates worsening of your condition.
The great part about the McKenzie Method is that it is a partnership. Your physiotherapist will work together with you and listen to your input. A movement will be tested and repeated in clinic to determine if it is safe to try for 3-7 days. You would then return to see if there has been improvement in how you feel and by testing strength and range of motion. Through conversation and testing during your sessions, you can find patterns that will provide clues to the solution of the problem. One example of these patterns includes centralization and peripheralization.
Centralization/Peripheralization
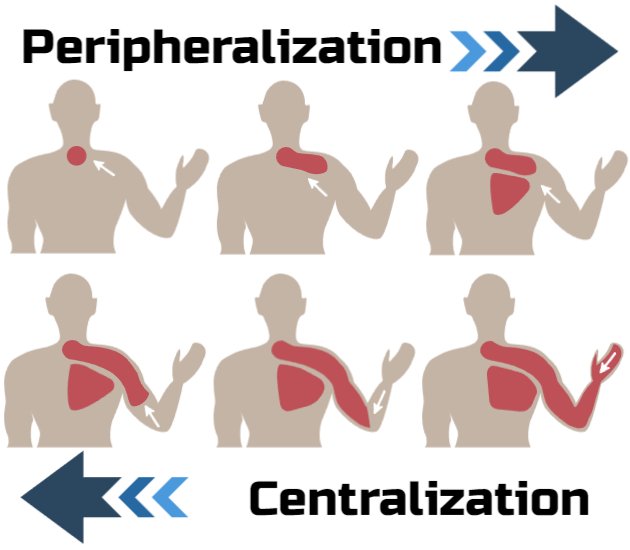
This is a well-researched phenomenon that happens with lower back injuries. Centralization and peripheralization both describe where your pain is moving. For example, peripheralization is where your leg pain travels down towards your feet. Centralization describes when your leg symptoms move towards the spine. In our case with lateral shifts, if your physiotherapist provides a movement and centralization occurs, you are both on the right track. But if your pain peripheralizes, this indicates that the movement provided may be irritating your injury. The picture below best illustrates centralization and peripheralization. For more information on centralization and peripheralization, check out this blog!
Still confused? Let me give you an example of a client who had a lateral shift:
Max is a 40-year-old male, who is an owner of a small construction company. He had developed back pain by doing some yard work lifting mulch. He bent forward while twisting and immediately experienced pain in his back and shooting left leg pain. He stopped everything he was doing and rested in bed until the next morning. Upon rising, he noticed stiffness in his back, tingling, burning and numbness down the left side of his leg. His wife, being extremely concerned, called his family doctor who prescribed Naproxen, providing some relief. Over the next couple of days, he noticed that his leg pain was less intense but constant. When looking in the mirror, he noticed that his shoulders were shifted to the right and hips to the left. He was unable to sit and had trouble bending forward. He called his family doctor again who ordered x-rays showing nothing remarkable.
Several weeks have gone by with no large changes. Max has found that lying down provides the most relief and standing improves his leg symptoms for short periods. When walking, he notices that his leg pain intensifies and travels down his left leg and toes. Max becomes increasingly more frustrated because he cannot walk the dog or help his wife with chores around the house. Sitting is painful and he is unable to lift anything because he can’t bend forward. He has taken time off work because it hurts too much to sit. He begins looking for help elsewhere. Massage therapy increases his pain and he cannot tolerate lying on his stomach and chiropractic adjustments make his leg pain worse that evening and into the next day.
We see this story commonly at Break Free. The question is what can we do to help?
Max started physiotherapy and an in-depth analysis was completed where the physiotherapist asked very specific questions about his injury. Some of the questions include how he hurt his back, the location of pain, what makes his symptoms better and worse and what his goals are.
During the physical examination, we found that his left big toe was weak indicating that there was compression at the L5 nerve root. There was diminished sensation along the outside of his left leg down to his pinky toe. We found that lying down on his stomach was quite painful. We noticed that he was visibly shifted to the right in standing, meaning his shoulders were over to the right and hips left. When we manually corrected the shift, it would produce pain in his leg but eventually improve. After several sessions of providing him with one specific movement at a time, his shoulders returned to their original resting position and he was no longer shifted. Max started to notice intermittent pain instead of constant left leg pain. The pain was no longer in his foot but in his upper thigh. With more physiotherapy the pain continued to travel towards the center of his back before it dissipated. He was eventually able to walk around the block and as time progressed, he was back to walking the dog. We provided strengthening of the lower back and education on lifting mechanics so he could return to gardening without aggravating his original back problem. He was also able to sit in a chair again and gradually returned to work.
Does this story sound similar to yours? If so, we want to help. Break Free Physiotherapy and Wellness is a team of physiotherapists trained in the McKenzie Method who would be happy to help you with your lateral shift. Book with one of skilled movement specialists who will listen to your story and help you find the exact movement to treat the source of your problem.
References
1. Laslett M. Manual correction of an acute lumbar lateral shift: maintenance of correction and rehabilitation: a case report with video. J Man Manip Ther. 2009;17(2):78-85. doi: 10.1179/106698109790824749. PMID: 20046549; PMCID: PMC2700497.
Corey Kim
Physiotherapist
Hey, my name is Corey, and I’m a co-owner of Break Free Physiotherapy and Wellness. I was born in Seoul, South Korea but grew up in London, Ontario. I finished both my Bachelor of Arts in Kinesiology and Master of Physical Therapy degrees at Western University. I’m passionate about helping people find pain relief through movement and believe in self-empowerment by sharing knowledge of the human body and its ability to heal. [full bio]