Causes of Knee Pain in Children
10 reasons for knee pain in children
Knee pain is a common condition that affects many children who are active. Children suffering from an injury are limited in their ability to stay active and participate in sports. The location of knee pain can vary based on the source of the problem, so it’s important to understand different parts of the knee that can be injured, and factors that increase the risk of certain problems.
1. Patellofemoral Pain Syndrome (PFPS)
One of the more common conditions for knee pain is patellofemoral pain syndrome. The location of pain with PFPS is the front of the knee around the knee cap (patella). The underside of the knee cap sits in a groove of the knee joint and glides smoothly when bending your knee. Due to muscular imbalances and tight muscles, the cartilage on the underside of the knee cap becomes irritated with increased use causing pain with running, jumping, descending stairs or rising from sitting.
For more information on Patellofemoral Pain Syndrome check out our PFPS Blog!
2. Osgood Schlatter’s Disease
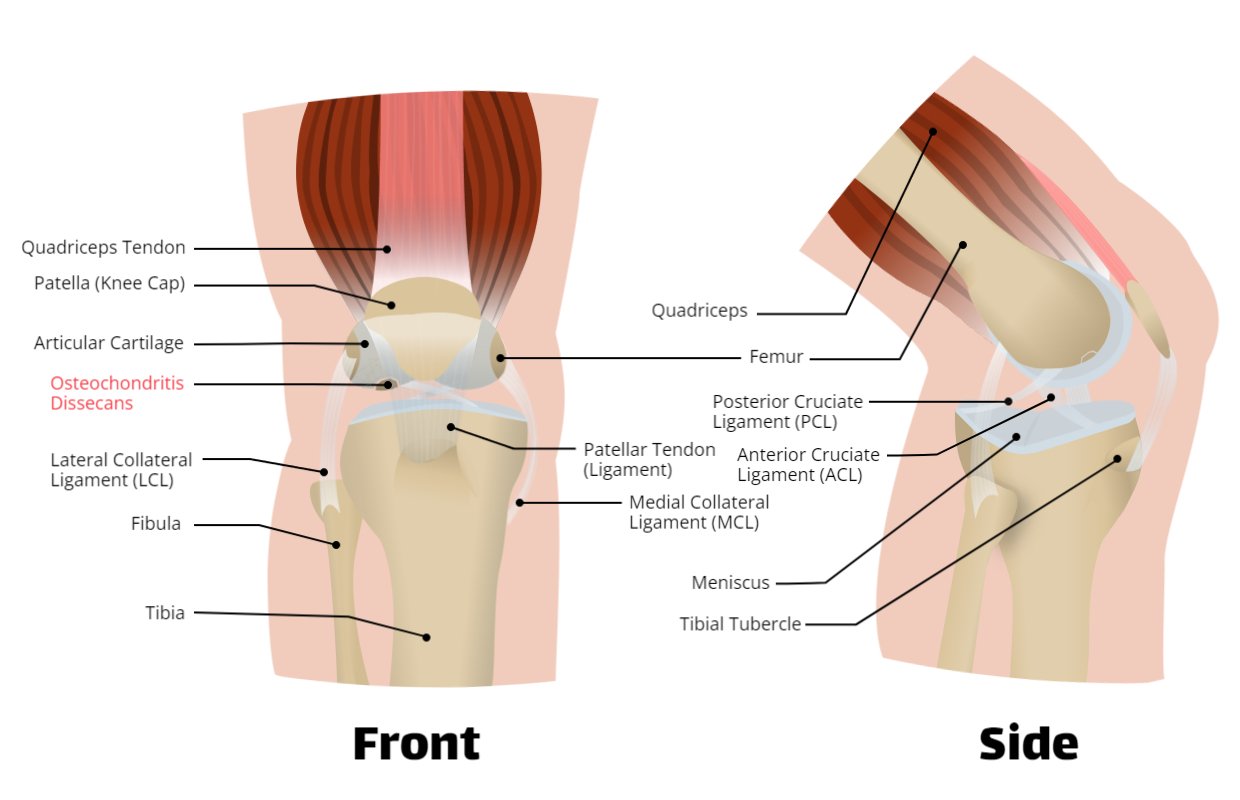
This diagram depicts the ligaments in your knee.
(Extra space has been added to assist with ligament visibility.)
This is a common problem in children who jump often. Also known as jumper’s knee, Osgood Schlatter’s Disease causes knee pain in the upper shin bone. The shin bone (also known as the tibia) has a bony prominence called the tibial tubercle. A tendon attaches to the tubercle and the knee cap. With excessive jumping, the tendon pulls away from the tibial tubercle causing pain. A common report is that it is tender to the touch, and gets worse with running, jumping and squatting repeatedly. It occurs when there is a sudden increase in jumping activities or weight bearing with certain exercises.
3. Patellar Dislocation
A patellar dislocation is when the knee cap moves out of the groove of the knee joint. It usually occurs when someone plants and twists, falls, or during a collision with another athlete in sport. Females are more likely to have this condition. Symptoms to look out for are a pop followed by swelling and pain in the knee cap area. In other cases, the knee cap will look out of place. Common risk factors include having previous dislocations, wider hip angles, and ligament laxity disorders. It’s important to have a proper assessment with a health care provider to determine if your child requires bracing. Physiotherapy is often the best tool to help treat this injury, but when patellar dislocations continue to recur, a consult with a specialist will be required.
4. ACL Injuries
ACL stands for anterior cruciate ligament and is one of the two ligaments inside of the knee. It prevents your tibia from moving forward, and provides stability in the knee. With the rise of children competing in competitive sports, ACL injuries have become more common in children and adolescents. The reported symptoms are giving way of the knee, or feeling unstable. Your physiotherapist will be able to complete special tests to determine if your child’s ACL is injured and requires physiotherapy treatment, or a specialist appointment.
5. MCL Injuries
MCL stands for medial collateral ligament, and is a ligament that supports the inside of the knee. It attaches to the femur and tibia, and helps provide stability with side-to-side movements. This ligament is injured with planting and twisting, sudden changes in direction while running, jumping with your knee moving inwards, or an impact on the outside of the knee. It is a common injury in soccer, football, basketball, skiing and tennis. A common complaint your child may have is that the inside of their knee hurts, or their knee feels unstable. Swelling, stiffness and tenderness to touch are also reported. Physiotherapists are trained to complete special tests to figure out the severity of the injury.
6. LCL Injuries
LCL is short for lateral collateral ligament, which is a less common location for injury. It is a ligament that supports the outside portion of your knee, connecting the femur to the tibia. This injury occurs when your child’s knee moves outwards with extra force, or suffers a direct blow to the inside of the knee. Quick turns can also cause this injury to worsen, which are more common in contact sports. Signs that your child might have this injury is pain on the outside portion of the knee, feeling of giving way, swelling, pain, and even sometimes numbness on the outside of the foot. This is because there are nerves that travel down the outside portion of the leg and knee.
7. PCL Injuries
PCL stands for posterior cruciate ligament, an internal ligament that is less commonly injured than the ACL. This ligament is responsible for preventing the shin bone from sliding behind the thighbone, and helps maintain stability of the knee. A blow to the front of the knee, or falling on a bent knee can cause injury to the PCL. It’s more likely to happen in sports such as basketball and soccer.
8. Patellar Tendinopathy
The patellar tendon attaches the knee cap to the shin bone. Pain in this tendon is often a sign of overuse, such as repetitive jumping. The most common symptoms reported are tenderness to touch, and pain during any movement that stretches the tendon. Quick contractions of the quadriceps muscle from sprinting, running and jumping may worsen symptoms. It’s described as a constant or intermittent ache.
9. Osteochondritis Dissecans
An injury that affects the joint and can happen in elbows and ankles, but most commonly in the knee. Osteochondritis dissecans is when a piece of the bone fully separates from the bone at the joint. The most common area for this to occur is at the end of the thighbone (femur) at the knee joint. Symptoms that are present with this injury include pain, swelling, locking or catching of the knee, or a sensation of giving way. Another symptom is changes in range of motion that are not consistent. It often occurs due to repetitive stress to the knee, or a genetic disposition. An x-ray or MRI may be warranted to confirm if your child has osteochondritis dissecans. Some cases resolve with physiotherapy, but other cases require a referral to a surgeon.
10. Juvenile Idiopathic Arthritis
JIA is a type of autoimmune or inflammatory condition in children under the age of 16. It is a condition in which the immune system (the one that fights off germs and viruses) attacks healthy tissue. This will cause swelling, pain, and tenderness in different joints in the body. These joints include hands, knees, ankles, elbows and/or wrists. Some symptoms of JIA include fatigue, blurry vision or dry eyes, rashes, appetite loss, and high fever. Special blood tests can be done to help confirm if your child has this condition. This includes testing erythrocyte sedimentation rate, c-reactive protein, rheumatoid factor, and complete blood count. Your family doctor, pediatrician or rheumatologist can order bloodwork and also order imaging such as X-Rays, MRI, or CT scans depending on the body part and condition. Physiotherapists are trained to provide a detailed assessment so that you are sent to the right specialist. They are also trained to help provide the right exercises for your child with JIA.
How do physiotherapists help children with knee pain?
There are a variety of reasons why your child’s knee may be sore, so getting professional help to diagnose the root cause is very important. A physiotherapist is a trained healthcare professional that has expertise in the field of musculoskeletal injuries. Here are a few reasons how physiotherapists can help.
1. Finding the Source of Your Problem
Physiotherapists are trained to understand how the body functions through movement. Based on your health history and your reports of where it hurts, physiotherapists are able to find out where the underlying problem is and how to treat it. By understanding your child’s injury through objective tests, your physiotherapist will be able to provide the exact stretch or exercise to help solve your child’s knee pain.
2. Exercise Therapy
Your child may have an underlying weakness that needs to be strengthened. As stated earlier, your physiotherapist is trained to determine which part of the knee is weak. This may include strengthening muscles above and below the knee to help take pressure off of the sore part of your knee.
3. Movement Mechanics and Form
In many cases of knee injuries with children, form or movement mechanics can be an issue when they participate in exercises. Your physiotherapist is trained to find these compensatory patterns, and provide coaching on how to decrease their pain when they jump or squat.
4. Active Rest
Sometimes your physiotherapist will provide specific instructions to either rest, or participate in another activity that won’t put stress on the knee. An example is biking as an alternative to running if your child has knee pain whilst running.
5. Bracing
Perhaps your child requires a brace to take pressure of the irritated structure of their knee. This will often help decrease overall pain and improve function if it is the correct brace. Bracing can help your child become more aware of what they are doing with their knee during activities. It may also cue your child to be careful when participating in sports or playing with their friends.
6. Education and Self-Management
We are in the business to help people find long term solutions so they can stay healthy and prevent injury! That includes teaching you and your child about their injury, what it is, and how to treat it yourself with some help and guidance from us! We provide the tools to heal and guidance along the path to recovery. We want both you and your child to understand what is happening to their knees. Understanding is the beginning of healing!
If your child is experiencing knee pain, and you’d like to determine the source and solution, call or email us now to book an initial assessment, or Book Online!